THE MATERNAL LYING-IN WARD
The lying-in ward is a division in the maternity ward where pregnant women who have given birth either by caesarean or by natural birth are placed under observation until they are discharged.
For pregnant women who had spontaneous delivery (natural birth), the observation is done for both the mother and the baby. The uterus is checked whether it is has contracted again and if there are any signs of the woman bleeding. The mothers are taught how to breastfeed their babies. The vital signs of the mother such as pulse, temperature, respiration and blood pressure are monitored.
Observation for the baby, its umbilical cord is checked for any signs of bleeding. After birth the baby needs to pass his first stool and urine if it hasn’t then there is the need for immediate surgery to help the baby pass out its first stool and urine. The baby’s sucking reflexes are checked. Most normal babies know how to feed unlike premature babies who have to be taught. The skin color of the baby is checked for cyanosis (lack of oxygen).
For women who have had caesarean operation, there is an additional observation after the general observation which is for both the mother and the baby. The incision site where she was operated is checked for any signs of bleeding. The fluids given to the mother is checked to ensure that the quantity being admitted into her body is equal to the quantity passing out of her body. Antibiotics is given to the woman to protect the incision site from any infection.
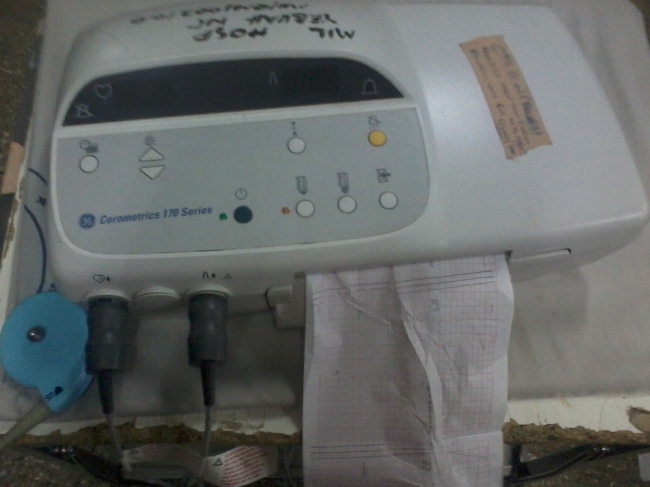
For anti-postpartum cases i.e. women who are not due for delivery. Women with high blood pressure and hypertension are observed and anti-hypertensive and anti-convulsant drugs are administered unto them. Women who are not due for delivery are not supposed to bleed, bleeding during pregnancy calls for immediate medical attention since one can lose the baby. The urine, protein of the mother is checked and the baby’s fetal rate is also checked.
In conclusion, women who have given birth by spontaneous vaginal delivery are discharged after six hours of observation. Women who have given birth by caesarean are observed for three days until they are discharged and women who are not yet due can be discharged after few hours of observation.http://youtu.be/Vt7E-ITkSMg



 </<a
</<a 